Oocyte Donation Program
A total of 153 oocytes were warmed and 134 survived. A total of 117 fertilized and 68% developed to blastocyst stage. A total of 47 embryos were transferred (2.35 embryos per recipient) and 26 implanted.
Oocyte Vs Egg
Fifteen patients achieved ongoing pregnancies initially, and two additional pregnancies were obtained after transfer of supernumerary vitrified/warmed embryos. Nine of the 10 donors from the current study had previous fresh donations cycles from where seven clinical pregnancies were established in nine recipients, providing the base for comparison. In the frame of this prospective study, oocytes were obtained from 10, all but 1, previously proven egg donors. All donors were healthy women under the age 35 years, and were screened and tested according to regulations ( x 25 Food and Drug Administration.
Inspection and enforcement; final rule. Federal Registry. Current good tissue practice for human cell, tissue, and cellular and tissue based product establishments November 2004.) (25). This study has been approved by the corresponding institutional review boards, and all participants signed the corresponding consent forms.Controlled ovarian hyperstimulation was performed as follows.
On day 2 or 3 after menses, subcutaneous rFSH, follitropin beta (Follistim; Organon Pharmaceuticals USA Inc., Roseland, NJ) administration was started (after keeping the donors on an oral contraceptive for a minimum of 14 days). Ovarian stimulation was monitored by the measurement of serum E 2 concentration and by ultrasonographic assessment of follicle diameter every 1 to 2 days. Gonadotropin-releasing hormone antagonist (ganirelix acetate) treatment was started on day 6 or day 7 of rFSH administration and continued until hCG was given. The antagonist treatment began when the lead follicle was 12 mm. Recombinant hCG (250 μg subcutaneously; Ovidrel; Serono, Inc., Rockland, MA) was administered within 36 hours after the last dose of gonadotropin, when the patient had at least one follicle 18 mm, and half of the follicle cohort had a 14-mm or larger diameter. Oocyte retrieval was performed 36 hours after hCG administration, using transvaginal ultrasound guidance and under anesthesia. The collected oocytes were washed and incubated for 30 to 60 minutes, then were denuded by 30-second exposure of Cumulase (Halozyme therapeutics, San Diego, CA), followed by mechanical denudation.
Oocyte maturity was assessed by light microscopy evaluation; those that presented a polar body were categorized as mature (metaphase-II stage; MII) and were eligible for freezing. In the current study, only in vivo matured MII oocytes were used. The steps of the vitrification and warming procedures were as reported earlier ( x 24 Chang, C.C., Shapiro, D.B., Bernal, D.P., Wright, G., Kort, H.I., and Nagy, Z.P. Two successful pregnancies obtained following oocyte vitrification and embryo re-vitrification. Reprod Biomed Online.
2008;16: 346–349 ) (24), but briefly it was as follows. The oocytes were first equilibrated in 7.5% Ethylene Glycol (EG) and 7.5% dimethyl sulfoxide (DMSO) for 15 minutes and transferred into the vitrification solution containing 15% EG and 15% DMSO and 0.5 mol/L sucrose, using a minimal volume approach. The base medium used was HEPES-buffered embryo culture medium (Cooper/Sage, Bedminster, NJ) supplemented with 20% (v/v) serum protein substitute (Cooper/Sage). Oocytes were placed onto a fine polypropylene strip (Cryotop, Kitazato Bio Pharma Co., Japan). Oocyte warming was performed by serial dilutions as follows: 1.0 M, 0.5 M, and 0 M sucrose.Oocytes that survived were inseminated by intracytoplasmic sperm injection (ICSI) 2 to 3 hours after warming using sperm from the husband of the corresponding recipient. The procedure of ICSI was performed as reported earlier ( x 26 Nagy, Z.P., Liu, J., Joris, H., Bocken, G., Desmet, B., Van Ranst, H. The influence of the site of sperm deposition and mode of oolemma breakage at intracytoplasmic sperm injection on fertilization and embryo development rates.
1995;10: 3171–3177 ) (26), the only difference being that a narrower diameter of ICSI injection pipette was used to minimize any damage during microinjection (MIC-CUST-30; Humagen Fertility Diagnostics, Charlottesville, VA).The day after ICSI, oocytes were assessed for the presence of pronuclei, and those displaying two pronuclei and two polar bodies were cultured further. Embryos were cultured until day 5, when morphologic selection by light microscope was performed and two or a maximum of three blastocysts with the highest grades were selected for transfer. Supernumerary embryos with sufficient developmental and morphologic status were vitrified on day 5 or day 6.Recipients were eligible to participate in the study if they were already on the waiting list for oocyte or embryo donation (before this study, for reasons of previously failed cycles related to advanced maternal age and/or impaired ovarian reserve), and they agreed and signed the corresponding institutional review board consent. For those 20 recipients who participated in this initial study, all IVF-related charges were waived. Preparation of recipients was performed using a standard protocol of leuprolide acetate, estrogen, and progesterone. In brief, leuprolide acetate was started in the midluteal phase of the cycle previous to embryo transfer, at a daily dosage of 1 mg.
After confirming down-regulation, by measuring the serum estrogen and progesterone levels, estrogen was commenced using Estrace pills (micronized E 2; Bristol-Myers Squibb Co., Princeton, NJ) at 1 mg twice a day for 5 days, then increased to 2 mg twice a day for 4 days, and finally to 2 mg orally three times a day for 4 days. Endometrial thickness was monitored by transvaginal ultrasound and serum E 2 levels were measured every 2 to 4 days. On the 15th day (“cycle day 15”) after estrace start (with adequate endometrial thickness), Progesterone in Oil, 25 mg, was administered. The day after, Progesterone in Oil, 50 mg, was administered, and on that day oocyte warming was performed, followed by the ICSI insemination procedure. Baixar tres vezes amor dublado rmvb to avi. Progesterone in Oil, 50 mg, was then continued daily until the first pregnancy test. Additionally, 100 mg of doxycycline for 7 days, and 16 mg of methylprednisolone on a daily basis for 7 days was given, starting on the 16th day.
Oocyte Donation Program Application
Administration of leuprolide acetate was suspended the day before embryo transfer. The first ultrasound was performed 20 to 22 days after embryo transfer. A clinical pregnancy was defined as the presence of fetal cardiac activity on transvaginal ultrasound.
A total of 153 vitrified MII oocytes were warmed for the 20 recipients: a mean of 7.65 per recipient; a minimum of 4, and a maximum of 12. From those warmed oocytes, 134 survived (89%), an average of 6.7 per recipient (minimum three and maximum nine). All surviving oocytes were inseminated and 117 fertilized normally (87%; lowest fertilization was 60% and the highest 100%; half of the recipients had maximum fertilization).
A total of 115 zygotes were developing on day 3 (98%; all patients but two had 100% cleavage stage development). A total of 78 embryos developed to the blastocyst stage by day 5 (68%). There were 47 embryos selected for embryo transfer (an average of 2.4 embryos per recipient). Seven patients had three embryos transferred and 13 had two embryos transferred. There were a total of 31 supernumerary embryos with sufficient quality, which were frozen using a vitrification protocol. Initial hCG levels were positive and rising for 16 recipients; 4 recipients had negative hCG tests.
One of the patients with initially rising serum hCG had a decline after the third measurement, and later no fetal cardiac activity was detected. In 15 patients a total of 26 fetal cardiac activities were detected, corresponding to a 55.3% implantation rate. Six of the pregnancies were singleton, seven were twin, and two were triplet implantations. All pregnancies were uneventful and all 26 infants have been born.

One club foot was noted in a triplet delivery; no other major or minor alterations were detected. The details on each individual recipient are presented in Table 1. Table 1 Laboratory and clinical outcomes in the 20 frozen/warmed oocyte recipients cycles (oocytes were obtained from 10 donors).
RecipientOocytes warmedOocytes survived% SurvivedFerti-lized% FertilizedD3 Cleaved% D3 CleavedD5 Blastocyst% D5 BlastocystETHCGFCACRYO003603POS031002672POSPOSPOSPOS761002332POS051003603POSPOS61005833POSNEG151003602POS2NEGPOSNEGPOSNEGPOSPOS2POS2POS12Results from these frozen–thawed egg donor cycles were compared with those from the donors' prior fresh donation cycles. As mentioned, all donors but one had prior donation cycle(s).In the fresh donation cycles a total of 322 oocyte–cumulus complexes were obtained (average of 35.8 per cycle), and 182 of them were inseminated with ICSI (an average of 22.7 oocytes compared with 6.7 oocytes in the frozen oocyte cycle; Table 2). A total of 137 oocytes fertilized after ICSI normally in the fresh donation (a mean of 67%), and 117 out of 134 fertilized in the frozen oocyte group (a mean of 87%). Nineteen embryos were transferred and nine of them implanted in the fresh cycle compared with 26 out of 47 in the frozen oocyte cycles. Initially six patients become pregnant in the fresh cycles; however, one of the pregnancies was an ectopic; thus, only five were ongoing in the nine recipients. A mean of 17.3 (a total of 156, including conventionally inseminated eggs) embryos were cryopreserved in the fresh cycles compared with the mean of 1.6 in the frozen oocyte cycles (a total of 31).
In both groups, there were two additional recipients who achieved pregnancies after transferring frozen/thawed (warmed) embryos; thus, the total pregnancy rate was 78% following fresh oocyte donation (a total of seven patients had clinical pregnancy out of the nine donation cycles), whereas a total of 17 patients achieved clinical pregnancy after frozen/warmed oocyte donation cycles (total pregnancy rate of 85%; Table 2). Table 2 Laboratory and clinical outcomes in the vitrified/warmed oocyte group with 10 donors and corresponding data of the same donors in their last fresh oocyte donation cycle.Cryo oocyteFresh oocytePNumber of donors109NANumber of recipients209NAMean age (±SD) of recipients39.7 (±4.8)39.6 (±5.8)NSMean number of oocytes per recipients7.735.8.
Egg Donation Program
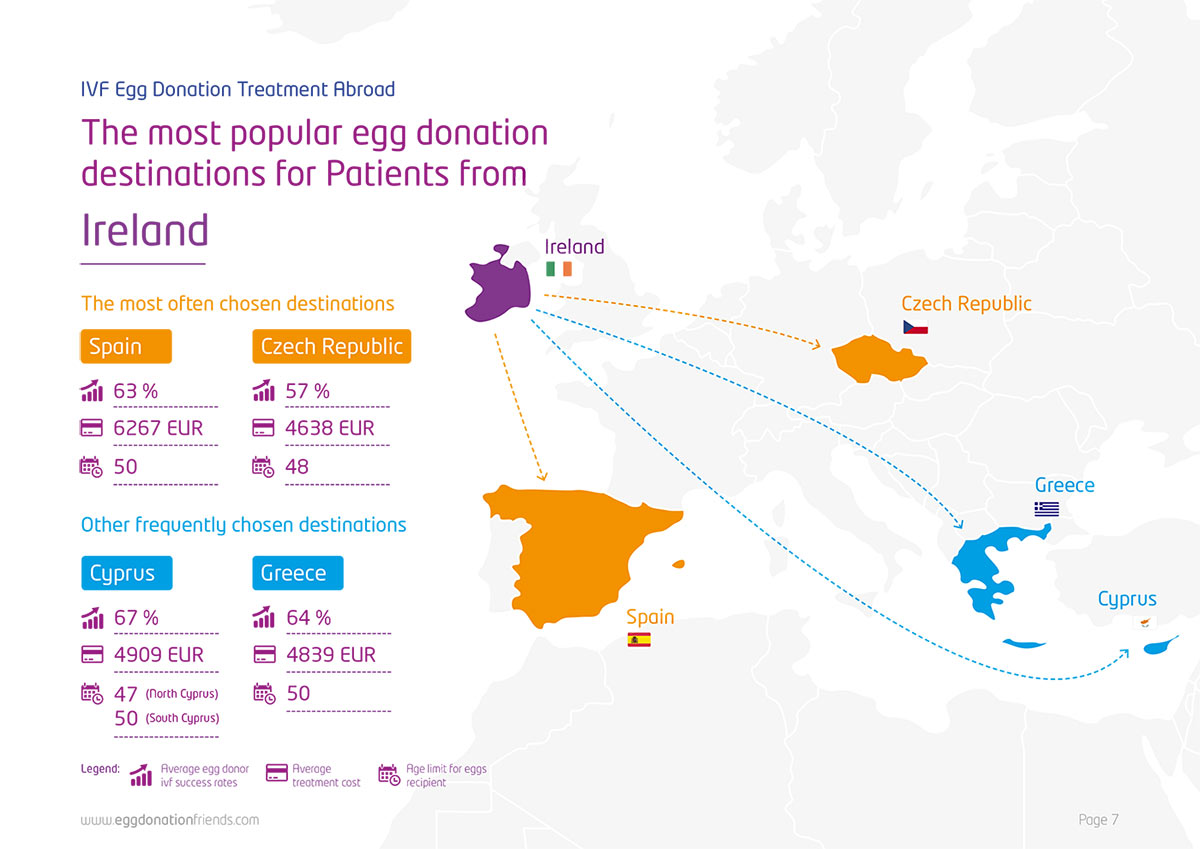
“Manor Medical Center” has developed an IVF program with oocyte donation, which is unique to Israel. This program provides you with everything you might require in such a delicate matter. Here are some highlights: Air transportation of fresh and frozen embryos to Israel Ability to receive up-to-date details on prospective oocyte donors Rigorous donor screening Israeli laboratory’s cutting-edge technology Affordable prices and convenient payment terms Emotional support Monthly treatment cycles Highly qualified, skilled personnel dedicated to providing professional patient-focused care. Your treatment program is highly customized and is designed with your preferences in mind. We take pride in our high success rate (60%).No need to fly to the Czech Republic, Cyprus or any other country and start a long and tedious journey, the end of which (unlike the beginning) is never certain.No need to rely on local personnel abroad and on unknown laboratories.